
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1403
Research Article(ISSN: 2644-1403) 
Association of Restrictive and Obstructive Lung Pattern on Post-Operative Pulmonary Complications After Cardiac Surgery: A Prospective Cohort Study Volume 4 - Issue 3
Mahsa Mirdamadi*
- Respiratory Disease Department, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Tehran, Iran
Received:June 7, 2021; Published: June 16, 2021
Corresponding author: Mahsa Mirdamadi, Respiratory Disease Department, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Tehran, Iran
DOI: 10.32474/GJAPM.2021.04.000189
Abstract
Background: About 38% of U.S. adults use prescription opioids. Opioid-related overdoses have risen in the last decade. Studies suggest that duration and type of first opioid prescribed play a significant role towards risky and chronic opioid use. Objective: The primary objective was to identify key players involved with initiation of patients on opioids. This study also identified patient characteristics most likely to receive care from influential opioid providers as opioid initiation interventions could be directed to such physicians.
Design/Participants: A cohort of patients with incident opioid use were identified using Arkansas All-Payer Claims Database from 2013-2018. A social network comprising provider as nodes and referrals as edges was constructed based on healthcare utilization 180 and 90 days preceding incident opioid use for potentially non-acute and potentially acute pain patients respectively.
Main Measures: Network centrality measures such as indegree (referrals received), eigenvector (neighbor centrality), betweenness (involvement) and closeness (reach) were estimated. Outcomes included influential providers determined by network centrality measures, initial opioid providers, and patients of influential providers. Covariates included provider demographics, patient demographics and clinical characteristics. Generalized linear mixed effect models were used for statistical analyses.
Key Results: There were 150,676 incident opioid users who visited 12,629 healthcare providers. Primary care providers (PCPs) were found to have higher centralities except for betweenness. Initial opioid prescribers showed higher network centralities. More complex patients such as those with more pain conditions and higher levels of comorbidity were more likely to seek opioid providers at the periphery of the network (lower indegree and eigen centrality).
Conclusions: This study highlights the characteristics of networks leading to opioid use. Findings that PCPs have higher influence and higher influence of initial opioid prescribers can guide opioid initiation guidelines as targeted interventions. Moreover, efforts should be undertaken to direct patients requiring judicious opioid prescribing to influential providers.
Keywords: Opioids; physicians; social network analysis; centrality.
Background
Patients with pulmonary disease either obstructive or restrictive lung pattern, in comparison with normal patients may have more intraoperative or post-operative pulmonary complications (PPCs). There is a concern that these kinds of pulmonary disorders may lead to prolonged length of stay (LOS) in hospital and even increase in death rate. Regardless of the type of surgery, PPCs when happen, may prolong hospitalization time [1]. In another study, restrictive pattern on spirometry was associated with a statistically significant increase in mortality after coronary artery bypass grafting (CABG). In this study trend was towards increased incidence of postoperative MI and longer hospital LOS [2]. In another study risk of postoperative pulmonary complications in patients undergoing thoracic or non-thoracic surgery in patients with interstitial lung disease (ILD) population was elevated Lawrence et al. [3] suggested that the severity of airways obstruction as measured by spirometry may not be an independent predictor of pulmonary complications even in high-risk procedures [4] Our study in cardiac valve surgery patients and in another unpublished study in all cardiac surgery showed the same result [5]. In one study the higher postoperative mortality rate in patients with severe COPD, CABG was solely accounted for post operation complication [6]. Despite presence of several study in this field, the correlation between groups with obstructive, restrictive and normal pattern in spirometry before cardiac surgery with PPC are not clear. In this article we are going to evaluate these relationships.
Methods and Materials
Study Design
This cross-sectional prospective cohort study designed to determine the incidence of pulmonary complications after cardiac surgery in patients with pulmonary abnormality. During 6 months from September 2016 to Mach 2017 all consecutive adult patients more than 18 years of age, who were candidates for CABG, congenital heart surgeries, or valve surgery in Rajaei Cardiovascular Medical and Research Center were enrolled. All patients had lab evaluation and spirometry measurement before surgery and followed during admition time with no further intervention. Emergency surgeries were excluded. We followed Helsinki protocol and our local ethical committee approved the study. Also, Iran University of Medical Sciences covered all expenses.
Demographic Data
History of comorbid diseases such as pulmonary function tests, presence of diabetes mellitus, renal failure, respiratory disease, and laboratory tests of patients were obtained from their documents or were asked directly from patients. Complete history, vital signs and clinical examination, chest X-ray, pulse oximetry, electrocardiogram, echocardiography, and complete blood test were taken, as a routine practice, to detect patient’s status. Arterial blood gas obtained through the arterial access line, on room air and then after 15 minutes giving 100% oxygenation while on ventilator, and recorded in a special sheet. All of patients received general anesthesia and put on pump oxygenator during surgery, as it is routinely done at our hospital. All surgeries were done via median sternotomy. Cold blood cardioplegin was used for cardiac arrest. At our intensive care unit (ICU), the patients are routinely extubated when they are hemodynamically stable and able to breathe adequately. After extubation, oxygen saturation (SPO2) is maintained above 90% by supplemental oxygen through the mask or nasal cannula, and patients could leave their bed as soon as general condition and patients tubing allowed. Further special evaluation was provided if the patient had complications requiring diagnostic tests or procedures based on specialist consult. To obtain the amount of total incidence of complications, the frequency of all morbidity in 24, 48, 72 hours after surgery, after leaving the ICU and finally before discharge from hospital were summed. All radiography and CT reviewed by our expert pulmonologists [7,8].
Patient Groups
Based on American Thoracic Society (ATS) statement, all patients with Forced Expiratory Volume to Forced Vital Capacity (FEV1/FVC) below 5th percentile of Lower Limit of Normal (LLN) considered as obstructive flow limitation (Obstructive Group). A restrictive lung defect is characterized by a reduction in FVC below the 5th percentile of the predicted value, and a normal or higher than normal FEV1/VC. Normal FEV1 and FVC and FEV1/FVC above 5th percentile characterized as Normal (normal group). We tried to match patients in “Normal Group” with “Restrictive and Obstructive Groups” based on age, gender and body mass index (BMI). Pattern and kinds of PPC compared across these groups and evaluated statistically.
Complication Definition
Pleural effusion (PE): PE was diagnosed based on Chest X-Ray (CXR) if blunting of costophrenic angle and loss of sharp silhouette of the ipsilateral hemidiaphragm in upright position, displacement of adjacent anatomical structures, or (in supine position) hazy opacity in one hemithorax with preserved vascular shadows [9-11] and also effusion need pleural catheter and evacuation. Effusion on CT, echocardiography and sonography also included as pleural effusion if this procedure was done for other reason and showed effusion in pleural space even if effusion not depicted in chest radiography.
Pneumonia: It was diagnosed by CXR with at least one of the following: infiltrate, consolidation, cavitation; plus at least one of the following: fever >38 °C with no other cause, white cell count <4 or >12×109, >70yr of age with altered mental status with no other cause; plus at least two of the following: new purulent/changed sputum, increased secretions/suctioning, new/worse cough/ dyspnoea/tachypnoea, rales/ bronchial breath sounds, worsening gas exchange. [9-11]
Hospital Acquired Pneumonia (HAP) or Ventilator Associated Pneumonia (VAP): Pneumonia either HAP or VAP diagnosis, were based on presence of new pulmonary infiltrates on chest X ray or CT scan, fever, cough or sputum after operation and if antibiotic started for pulmonary infiltrate based on diagnosis of pulmonologist or infectious specialist. Leukocytosis is common after these kinds of cardiac operations, and we considered HAP in our patients if they had at least two or more of the above findings plus leukocytosis. VAP was accepted if the patient remained intubated more than 48 hours and had other criteria of pneumonia. Diaphragm Dysfunction or Paralysis: It was diagnosed if significant permanent diaphragm elevation was seen on CXR and/ or ultrasonography approved decreased or absence of diaphragm muscles contraction. Phrenic nerve conduction velocity (NCV) and diaphragm electromyogram (EMG) were not available at our center in ICU. All newfound, significant left diaphragm elevation, that persist in last radiography at discharge time considered as diaphragm paralysis even if no sonography or fluoroscopy is done for diagnosis.
Atelectasis: Lung opacification with mediastinal shift, hilum or hemidiaphragm shift towards the affected area, with compensatory hyperinflation in adjacent non-atelectatic lung19,20,21 Plate atelectasis, lobar, multi-lobar atelectasis and or whole lung collapse all categorized and considered as atelectasis.
Pneumothorax: Air in the pleural space with no vascular bed surrounding the visceral pleura.19,20,21 ARDS/Pulmonary Edema: Diagnosis of ARDS/Pulmonary Edema was based on radiographic findings and clinical condition of patient. It was impossible to follow Berlin definition of ARDS and therefore edema and ARDS considered as one entity.
Statistical Analysis: Results are presented as mean ± standard deviation (SD), or frequencies with percentages, as appropriate. Comparisons across groups were made with one-way analysis of variance (ANOVA), chi-square test, chi-square test for trend, or Fisher’s exact test as appropriate. No statistically significant skewness was met in frequency distribution of numeric variables (p>0.05). All analyses were performed using SPSS version 19.0 software (SPSS, Inc., Chicago, IL). A 2-tailed p-value of ≤0.05 was considered statistically significant.
Results
In this study Groups of patients classified and homogenized to reduce influence of other confounding factors. As we can see in Table 1, all patients’ groups are matched for age, gender and BMI. Demographic, historical and laboratory characteristics of the subjects in each of obstructive, restrictive, and normal pulmonary conditions according to the ATS statement are shown in Table 1.
a. As can be seen in Table 1, the mean of age and BMI and the frequency distribution of gender are not statistically different across the three groups (p>0.05), as we attempted to match groups according to age, BMI and gender. History of morning fatigue was more common in restrictive patients (p=0.010). Also, restrictive patients had higher eGFR and FBS than patients with other pulmonary conditions (p=0.016 and p=0.011, respectively). Obstructive patients had higher creatinine level and less likely to be ASA class 1 and 2 compared to restrictive and normal subjects (p=0.002 and p<0.001, respectively). However, hypertension was more prevalent in obstructive patients, but it did not reach statistically significant difference (p=0.083). The rest of demographic, historical and laboratory characteristics did not statistically differ across the three groups (p>0.05) Table 1. Spirometric values of the subjects are depicted in Table 1.
b. As can be seen, the level of both FEV1(mv) and FEV1(PP) are increased in normal subjects than in pulmonary patients (p<0.001). FVC (mv) and FVC(PP) levels showed reduction in restrictive patients compared to other groups (p<0.001). The level of FEV1/FVC(PP) and PEFR (PP) were statistically different across the three groups (p<0.001). The mean of MMEF was lowered in obstructive patients than in either group restrictive of normal (p<0.001) Table 2. Intraoperative characteristics of subjects are abstracted in Table 3. In obstructive patients, PO2_100 showed highly increase in normal patients compared to restrictive and normal subjects (p<0.001). Mechanical ventilation time tended to be statistically different among groups (p=0.059). The mean of PO2_air was lowered in obstructive patients than in either groups restrictive or normal (p<0.021), while none of the other intraoperative characteristics was statistically different across the three groups (p>0.05) Table 3. Table 4 demonstrates postoperative complications among the three groups. PE and ARDS was very less common in obstructive patients than in restrictive and normal subjects (p=0.010). The frequency of other post-operative complications was not statistically different among study groups (p>0.05). Table 5 suggests that there were no significant differences in outcomes across the three groups (p>0.05). In 623 subjects participated in this cross-sectional prospective cohort study, mortality was observed in just 15 cases (2.4%). The mean length of stay in ICU was about 3.5 days, length of stay in hospital was around 16 days, and intubation time was just 740 minutes Table 5.
Table 1: Demographic, historical, and laboratory characteristics of patients with obstructive, restrictive, and normal spirometry before cardiac surgery.

Data are presented as mean ± SD (standard deviation) or n(%). BMI; Body Mass Index, ESS; Epward Sleepiness Score, Hb; Hemoglobin, eGFR; estimated Glomerular Filtration Rate, Cr; Creatinine, FBS; Fasting Blood Sugar, SPAP; Systolic Pulmonary Arterial Pressure, TSH; Thyroid Stimulating Hormone, EF; Ejection Fraction, PO2 Air; Pressure of Oxygen in room air.
Data are presented as mean ± SD (standard deviation). MV; Measured Values, PP; Percent Predicted, FEV1; Forced Expiratory Volume at first second, FVC; Forced Vital Capacity, MMEF; Maximum Mid Expiratory Flow rate, PEFR; Peak Expiratory Flow
Table 3: Some intraoperative characteristics of patients with obstructive, restrictive, and normal spirometry at the time of cardiac surgery.
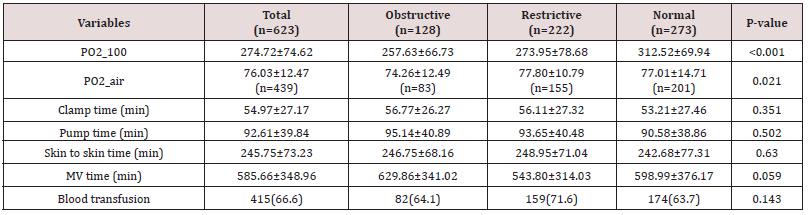
Data are presented as mean ± SD (standard deviation) or n(%). PO2_100; Arterial Pressure of Oxygen after taking 100 percent Oxygen, PO2_Air; Arterial Pressure of Oxygen on Room Air, MV time = Mechanical Ventilation
Table 4: Comparison of Post-operative complications in patients with obstructive, restrictive, and normal spirometry.

Data are presented as n(%). PE; Pulmonary Edema, ARDS; Adult Respiratory Distress Syndrome.
Table 5: Comparison of outcome of cardiac surgery in patients with obstructive, restrictive, and normal spirometry.
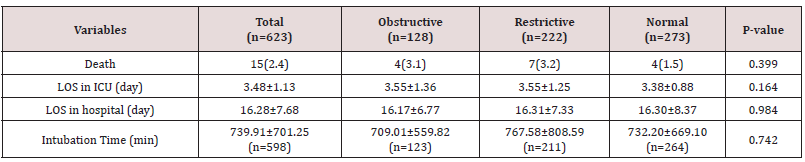
Data are presented as mean ± SD (standard deviation) or n(%). LOS; Length of Stay, ICU; Intensive Care Unit.
Discussion
By evaluation of PubMed and Google we found no study that compare patients with restrictive and obstructive lung disease regard to PPCs with normal patients. Cardiac surgery with pump perfusion is a high-risk surgery with significant PPCs and we are routinely encounter these complications in our center. In this study we are going to define prevalence of POPCs in all kinds of cardiac surgery and compare those patients with restrictive or obstructive airflow limitation with those with no known pulmonary disease and normal spirometry values. As it is obvious in Table 2, in regard to spirometry values we can show that because of categorization, all three groups of patients are significantly different, and we are comparing these groups from PPCs point of view. There are some pulmonary complications after non-emergency cardiac surgery but can be life threatening in rare cases. The documented incidence of PPCs ranges from 3% to 16% after CABG and 5%-7% after valvular heart surgery [9-12]. The reported frequency of pulmonary complications after cardiac surgery varies from 6% to 70% depending upon the criteria used to define pulmonary complications [13]. Furthermore, patients undergoing cardiac surgery often have underlying pulmonary illnesses such as obstructive lung disease (e.g., chronic obstructive pulmonary disease) and restrictive lung disease (e.g., congestive heart failure, and interstitial lung disease,) which may increase their susceptibility to postoperative respiratory problems. In our study, PPCs occurred in 362 (58.1%) patients after surgery, with 81 (63.3%) incidence in patients with obstructive lung pattern ,130 (58.6%) in patients with restrictive lung pattern and 151 (55.3%) in patient with normal lung pattern.
The incidence of PPCs in our study was comparable to the results of other international studies. Otherwise, incidence of pulmonary complications after cardiac surgery were not significantly different in patients with normal and abnormal pulmonary pattern. Main objective of this study was to compare patient with obstructive and restrictive pattern of flow limitation in spirometry with those with normal spirometry about PPC after all types of cardiac surgery, Length of stay in ICU and hospital (cost of operation), intubation time, and death of patient candidate for cardiac surgery. There were not any significant differences between those patients with normal and abnormal pulmonary function. Although the impact of severe lung disease such as COPD on patients undergoing cardiac surgery was traditionally considered potentially dangerous for cardiac surgery, we did not find any. About patients undergoing CABG, COPD was reported to be an independent risk factor for postoperative morbidity and/or mortality [14,15] However, because of the recent improvements in anesthesia, cardiac protection, and surgical techniques, as well as the advances in preoperative pulmonary evaluation and medical optimization, it becomes possible to perform CABG with acceptable morbidity and mortality rates in patients with highrisk. There are many studies have reported that patients with mild to moderate COPD or even severe COPD did not have a higher risk of postoperative mortality and morbidity rates than those without COPD [16-18] There were only two complications which was significantly different in these tree groups. We found pleural effusion and ARDS were very less common in obstructive patients than restrictive and normal subjects. This finding could be explained by the fact that more patient with heart failure and cardiomegaly might have been included in our restrictive group.
To compare pulmonary complication and in hospital outcomes of our patient in these three groups, we found no important difference among them. Pulmonary edema or ARDS showed statistically significant in these patients. Number of ARDS and Pulmonary edema was significantly higher in restrictive group in comparison with obstructive and normal groups. This finding could be explained by the fact that more patient with heart failure and cardiomegaly might have been included in this group. Evaluation of ejection fraction of this patient showed more patient with heart failure categorized in restrictive group. Some limitations should be considered when interpreting the results in the present study. First, this study was cohort, and publication bias cannot be avoided because of its nature. Second, because of no internationally unified criteria have existed until recently, the definition of obstructive and restrictive lung pattern in published studies was various. In the present study, only spirometric pattern confirmed by a FEV1/ FVC, FEV1, FVC, or by the diagnosis and/or treatment record were included. Although these inclusion criteria were aimed to diminish the potential bias in the lung disease definition, it might also induce bias in the results to some extent. Third, the included studies cover variety cardiac surgery (such as valvular, vascular cardiac surgery) and surgeon, during which variable surgery may occur in the operative and postoperative complications. These changes might affect the outcomes of interest [19,20].
Conclusion
Despite statistically significant correlation between high blood sugar, lower GFR, anemia and history of fatigue with PPCs, we found no statistically significant difference between obstructive, restrictive and normal groups, in regard to LOS in hospital and ICU and death.
References
- Srinivas R Bapoje, Julia Feliz Whitaker, Tara Schulz, Eugene S Chu, Richard K Albert (2007) Preoperative Evaluation of the Patient with Pulmonary Disease. CHEST 132: 1637-1645.
- Jonaid Aslam, Srikanth Vallurupalli, Abiy Kelil, Peter (2010) Outcomes After Coronary Artery Bypass Grafting in Patients with Restrictive Spirometry Pattern. 10602 October 138.
- Nina M Patel, Tejaswini Kulkarni, Daniel Dilling, Mary Beth Scholand (2019) Preoperative Evaluation of Patients with Interstitial Lung Disease. CHEST 156(5): 826-833.
- Lawrence VA, Page CP, Harris GD (1989) Preoperative spirometry before abdominal operations: a critical appraisal of its predictive value. Arch Intern Med 149: 280-285.
- Hasan Allah Sadeghi, Reza Alirezaye Tabrizi, Behshid Ghadrdoost, Rasoul Azarfarin (2017) Evaluation of Pulmonary Complications in Patients with Valvular Heart Surgery: Clinical and Laboratory Significances. Res Cardiovasc Med 6(2): e39944.
- Kurt Kroenke, Valerie A Lawrence, John F Theroux, Michael R Tuley, Susan Hilsenbeck (1993) Postoperative Complications After Thoracic and Major Abdominal Surgery in Patients with and Without Obstructive Lung Disease. Chest.
- Miskovic A, Lumb AB (2017) Postoperative pulmonary complications. British Journal of Anaesthesia 118(3): 317-334.
- Younossian A, Adler D, Bridevaux P, Kherad O (2011) Postoperative pulmonary complications: how to anticipate and prevent the risk? Rev Med Suisse 7(317): 2214,2216-2219.
- Canet J, Gallart L, Gomar C (2010) Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology 113: 1338-1350.
- Jeong BH, Shin B, Eom JS (2014) Development of a prediction rule for estimating postoperative pulmonary complications. PLoSOne 9: e113656.
- Mazo V, Sabate S, Canet J (2014) Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology 121: 219-231.
- Smetana GW (2009) Postoperative pulmonary complications: an update on risk assessment and reduction. Cleve Clin J Med 76(4): S60-S65.
- Sachdev G, Napolitano LM (2012) Postoperative pulmonary complications: pneumonia and acute respiratory failure. Surg Clin North Am 92(2): 321-344.
- Rock P, Rich PB (2003) Postoperative pulmonary complications. Curr Opin Anesthesiol 16(2): 123-131.
- Chumillas S, Ponce J, Delgado F, Viciano V, Mateu M (1998) Prevention of postoperative pulmonary complications through respiratory rehabilitation: a controlled clinical study. Arch Phys Med Rehabil. 79(1): 5-9.
- Magovern JA, Sakert T, Magovern GJ (1996) A model that predicts morbidity and mortality after coronary artery bypass graft surgery. J Am Coll Cardiol 28: 1147-1153.
- Higgins TL, Estafanous FG, Loop FD (1992) Stratification of morbidity and mortality outcome by preoperative risk factors in coronary artery bypass patients. A clinical severity scores. JAMA 267: 2344-2348.
- Samuels LE, Kaufman MS, Morris RJ (1998) Coronary artery bypass grafting in patients with COPD. Chest 113: 878-882.
- Angouras DC, Anagnostopoulos CE, Chamogeorgakis TP (2010) Postoperative and long- term outcome of patients with chronic obstructive pulmonary disease undergoing coronary artery bypass grafting. Ann Thorac Surg 89: 1112-1118.
- Michalopoulos A, Geroulanos S, Papadimitriou L (2001) Mild or moderate chronic obstructive pulmonary disease risk in elective coronary artery bypass grafting surgery. World J Surg 25: 1507-1511.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





